Abstract

Purpose
The treatment success in patients (pts) with acute myeloid leukemia (AML) is very heterogeneous. Especially for older pts considered unfit for intensive treatment incl. allogeneic stem cell transplantation (alloSCT), outcome remains poor. Hypomethylating agents such as 5-azacytidine (azacitidine) or 5-azadeoxycytidine (decitabine) improve overall survival (OS) compared to standard of care. In the context of conventional chemotherapy and even after alloSCT, TP53 mutations are one of the worst prognostic factors. Recently, Welch et al. published their results of a ten-day regimen of decitabine treatment showing that pts with a TP53 mutation had a similar OS and even higher response rates compared to those without this high-risk feature (N Engl J Med 2016;375:2023-36).
Here, we analysed a large, well characterized cohort of AML pts treated with decitabine and studied tThe impact of the TP53 mutation status on outcome.
Patients and Methods
All AML pts consecutively enrolled in the SAL registry or diagnosed at the University Hospital Graz and treated with decitabine between Nov. 2011 and Feb. 2017 were included in this analysis. The study was conducted in accordance to the Declaration of Helsinki and approved by the responsible ethics committee. Informed consent was obtained from all patients.
Next-generation sequencing (NGS) on an Illumina MiSeq-system was used to detect TP53 mutations using pre-treatment samples (bone marrow or peripheral blood in case of peripheral blasts). All samples with synonymous mutations or no detectable mutations according to the predefined cut-off of 10% were classified as TP53 wild type (wt).
OS and response to therapy was analysed for all pts and according to the mutational status. All time-dependent events were calculated from the start of decitabine treatment.
Results
Overall, data of 296 pts was analysed. Median age was 73 years (range, 20 to 94), 52% had de novo AML, 33% sAML and 15% therapy-related AML. Based on cytogenetics, 19% of pts were in the favorable risk category, 43% had intermediate and 23% adverse risk according to the 2017 ELN criteria. Nine percent had an FLT3-ITD mutation and 19% a mutated NPM1 .
One-hundred seventy one pts received decitabine as first-line therapy, the remaining pts were treated with decitabine as second-line or salvage therapy. Thirty-three pts were treated with ten day courses of decitabine as first-line therapy, all others received the standard five day regimen.
Overall, the rate of complete remission or CR with incomplete recovery (CR/CRi) was 12%. Thirty percent of pts achieved at least a partial remission (PR) or stable disease (SD), resulting in an overall response rate (ORR) of 42%.
With a median follow up of 22 months (IQR, 11.9 - 30.6) from start of decitabine treatment, the median OS for the whole cohort was 4.6 months (IQR, 2.0 - 11.1).
For those 171 pts receiving first-line treatment with decitabine, rates of CR/CRi were 16%, and 23% had PR or SD. The median OS was 5.9 months (IQR, 2.6 - 12.9 months). Median OS for pts with SD or better was 13.4 months (IQR, 8.2 - 26.4) compared to 4.0 months (IQR, 2.6 - 9.4) for those with no response.
Pts treated with a ten day regimen had higher CR/CRi rates (27%) and longer OS (13.4 months).
NGS based mutation screening was performed on samples of 180 pts with available pre-treatment material. TP53 mutations ( TP53 mut) were found in 20 pts (11%). As expected, pts with TP53 mut had more often adverse risk cytogenetics and lower frequencies of concomitant NPM1 mutations. No significant differences were observed for age, type of AML, and ECOG performance status. Among those 180 patients, three TP53 mut pts were treated with ten day regimen (15%) as opposed to 19 TP53 wt pts (12%).
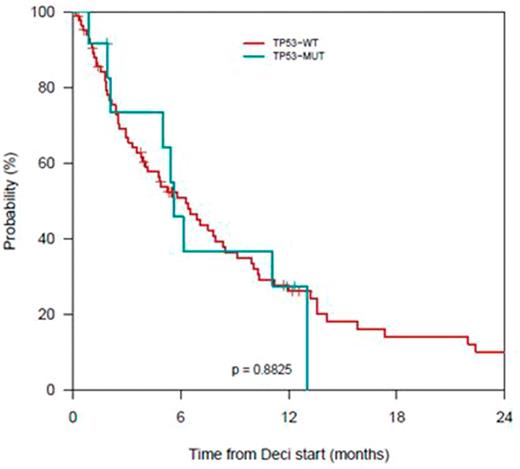
Response rates did no differ between TP53 wt pts (12% CR/CRi) and TP53 mut pts (15% CR/CRi, p =.45). Median OS was 4.9 months (IQR, 1.8 - 10.7) for TP53 wt pts and 5.4 months (IQR, 2.7 - 6.2) for TP53 mut pts ( p =.63). For those pts receiving first-line treatment with decitabine the corresponding numbers are 6.3 months (IQR, 2.4 - 13.2) for TP53 wt pts and 5.6 months (IQR, 2.1 - 13.1) for TP53 mut pts, respectively ( p =.88).
Conclusion
This analysis of a large cohort of AML pts shows response rates and OS after decitabine treatment in a real world setting. Interestingly, the prognosis was not negatively influenced by a TP53 mutation with the standard five-day regime of decitabine.
Fig. 1 OS for pts with decitabine first-line therapy acc. to TP53 mutation status
Rollig: Bayer: Research Funding; Janssen: Research Funding. Middeke: Janssen: Consultancy, Research Funding. Hochhaus: BMS: Research Funding; Incyte: Research Funding; Novartis: Research Funding; Pfizer: Research Funding; ARIAD: Research Funding; MSD: Research Funding. Brümmendorf: Takeda: Consultancy, Research Funding; Novartis: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding. Stoelzel: medac: Other: Travel support. Platzbecker: Celgene: Consultancy, Honoraria, Research Funding; Janssen: Consultancy, Honoraria, Research Funding; Acceleron: Consultancy, Honoraria, Research Funding; Novartis: Consultancy, Research Funding. Schetelig: Janssen: Consultancy, Honoraria; Abbvie: Honoraria; Roche: Honoraria; Sanofi Aventis: Consultancy, Research Funding. Thiede: Roche: Consultancy; Bayer: Consultancy, Speakers Bureau; Novartis: Consultancy, Speakers Bureau; Agendix: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal